
Receiver operating characteristic (ROC) curves were drawn to evaluate the feasibility and accuracy of CAN-RS in diabetic oculopathy screening.
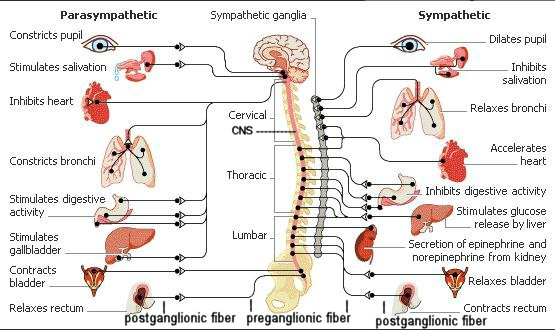
#AUTONOMIC NERVOUS SYSTEM LENS SKIN#
The electrochemical skin conductance (ESC) of the hands and feet was measured by SUDOSCAN, from which a cardiovascular autonomic neuropathy risk score (CAN-RS) was calculated.
#AUTONOMIC NERVOUS SYSTEM LENS PROFESSIONAL#
The state of visual acuity, the lens, the vitreous, and the fundus were tested by professional ophthalmic instruments. A total of 335 subjects with T2DM were enrolled. This study aims to explore the relationship between autonomic nerve dysfunction-assessed by cardiovascular autonomic neuropathy risk score (CAN-RS)-and ocular abnormality in Chinese type 2 diabetes mellitus (T2DM). Anyone experiencing these symptoms should see a doctor or ophthalmologist for a diagnosis.Objective. The symptoms of Adie syndrome are typically not severe or debilitating, but the condition can disrupt daily life and usually requires treatment. While the combination of decreased sweating, absent reflexes, and poor pupil responses is technically known as Ross’s syndrome, some doctors may diagnose this as a variant of Adie syndrome. In some cases, a person may experience changes in sweating, which can be either excessive or reduced. Some people may experience additional symptoms, including headaches, pain in the face, and mood swings. Examples include reflexes in the knee and Achilles tendon. Deep tendon reflexes are automatic, involuntary responses of the muscles in response to stimuli. In addition to symptoms in the eye, a person with Adie syndrome will also have sluggish or absent deep tendon reflexes.

However, they may eventually begin to affect both eyes. The symptoms of Adie syndrome tend to affect just one of the eyes. In other cases, symptoms such as light sensitivity or the presence of “light glares” within the field of vision may also occur. The vision may be blurry, for instance, or the person may have trouble with depth perception. However, some people may experience impaired vision. The affected eye may not necessarily cause symptoms. The eye may be less responsive, even when doctors shine a bright light near the eye to test for a reaction. The pupil may stay dilated, meaning that it is open wider than necessary in the presence of light. If a person has Adie syndrome, the affected pupil does not do this correctly. These changes happen very quickly to help humans see in different light conditions.
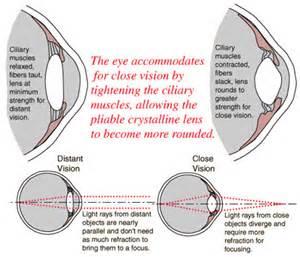
In general, the pupils get smaller or larger in response to changes in light. Typically, Adie syndrome may result in a change in the dilation of one of the pupils.

In these instances, it is possible to inherit the syndrome from a parent. In rare cases, causes of Adie syndrome may have a genetic aspect, as well. Damage to the dorsal root ganglion at the root of spinal nerves may have similar causes and could lead to a loss of reflex in these areas. The loss of deep tendon reflexes, such as the Achilles or patellar reflex, may also occur due to similar damage in the nerves. This inflammation or damage to the nerves may arise from issues such as: Symptoms may have their own mixed causes.Ī leading theory is that inflammation or nerve damage in the ciliary ganglion, which sits just behind the eye, causes symptoms in the eye, including the improperly dilated pupil. In most cases, Adie syndrome is idiopathic, which means that doctors do not know the exact cause. It is most common in young adults between the ages of 25 and 45 years and more likely to affect females than males. Share on Pinterest People with Adie syndrome have eyes that respond more slowly to light.Īdie syndrome is relatively rare, affecting close to 5 in every 100,000 people.


 0 kommentar(er)
0 kommentar(er)
